Influenza, commonly known as the flu, brings substantial health and economic burden every year in the United States and worldwide. According to the Centers for Disease Control and Prevention (CDC), the flu has resulted in 9-45 million illnesses, and 12,000-61,000 deaths annually in the U.S. since 2010. The total economic cost of influenza is estimated to be $11.2 billion per year in the country alone.
With effective vaccination coverage, communities can achieve immunity goal and protect the most vulnerable populations. Continued innovation and growth across the influenza vaccines market is crucial to improve protection against this high-risk respiratory virus.
Annually, the World Health Organization (WHO) meticulously selects the influenza virus strains for upcoming season’s vaccines based on extensive global surveillance data. This process aims to provide optimal protection against circulating influenza viruses by adjusting the strains included to match the predicted prevalent and threatening viruses. The recommended strains typically consist of two influenza A viruses and two influenza B viruses. By recommending specific combinations, the WHO ensures broad protection against potential culprits of seasonal influenza, potentially lessening illness, hospitalization, and mortality rates.
New Trends and Innovation
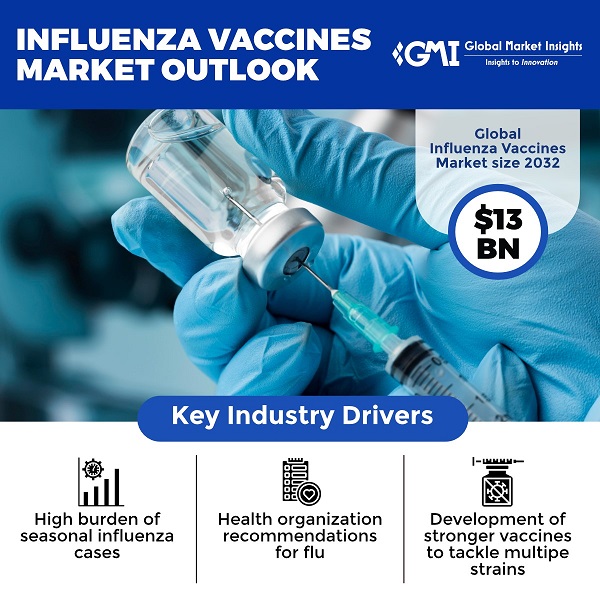
The influenza vaccines industry, which is expected to surpass US$13 billion in value by 2032, has seen several new trends and innovations in recent years, aimed at improving the effectiveness and accessibility of flu vaccines. Some key trends include:
High-Dose Vaccines
High-dose flu vaccines contain four times the amount of antigen as standard flu shots, aiming to provide better immunity for patients who may have a weaker immune response. Studies have found high-dose vaccines can reduce risk of flu infection in seniors compared to standard-dose shots. With support from organizations such as the WHO, global awareness and demand for high-dose flu shots is expected to grow steadily, while drug manufacturers working to bolster vaccine support and production.
According to study released by Kaiser Permanente Northern California in 2023, high-dose influenza vaccines could lower infections by nearly 15% as compared to standard-dose vaccines. Researchers immunized over 1.6 million patients aged 18 to 64 with high-dose quadrivalent flu vaccine or standard-dose vaccines in 2018-19 and 2019-20. In the 50 to 64 age group, 2.0 cases per 1,000 people were diagnosed with flu in the high-dose recombinant group, while 2.3 cases per 1,000 were diagnosed in the standard-dose group, resulting in a relative vaccine effectiveness (VE) of 15.3% (95% CI, 5.9% to 23.8%).
During April 2023, pharma giant Sanofi and U.S. government’s Biomedical Advanced Research and Development Authority confirmed the groundbreaking for a 2-storey facility in Pennsylvania, for making flu vaccines. The aim of the contract is to enhance readiness by utilizing the innovative recombinant, protein-based technology for distributing a pandemic vaccine. Sanofi produces Fluzone High-Dose, a quadrivalent vaccine designed to target four strains of influenza.
Adjuvanted Vaccines
Adjuvanted influenza vaccines have emerged as a promising trend in the field of flu vaccination, particularly for older adults who may have a weaker immune response to traditional vaccines. Adjuvants are ingredients added to some vaccines to boost the immune response and create longer-lasting immunity to influenza viruses. Adjuvanted flu vaccines are designed to work well in older adults or those with weaker immune systems.
According to a report on influenza vaccines market by Global Market Insights Inc., the share from adult segment will expand at approx. 7.3% CAGR up to 2032, indicating the significant and prospective demand for adjuvanted vaccines.
Researchers at the Institute for Biomedical Sciences at Georgia State University published a study last year on a protein nanoparticle vaccine with an adjuvant that improves the immune response against influenza. The study describes a promising vaccine candidate that utilizes adjuvants to enhance effectiveness against viral infections. The researchers hope that these adjuvanted protein nanoparticles could be used as mucosal vaccines, either alone or in combination with other vaccines to enhance mucosal immunity and protection.
Recent research on the Fluad quadrivalent vaccine, specifically designed to enhance immune responses and overcome immunosenescence in older adults, was published in 2023. Employing a static compartmental model aligned with CDC guidelines, the research project calculated the incremental reduction in influenza-related outcomes achieved by administering adjuvanted trivalent inactivated influenza vaccine (aIIV3) versus generic quadrivalent inactivated influenza vaccine (IIV4) among individuals aged 65 and above across three influenza seasons. The findings indicated that aIIV3 exhibited superior efficacy in mitigating influenza infections.
Cell-Based Influenza Vaccines
Most flu vaccines are produced by growing viruses in chicken eggs. Cell-based vaccines are produced by growing viruses in animal cells, viewed as a faster and more reliable production method. Cell-based vaccines may induce a stronger immune response. One major driver is the increasing demand for more efficient and reliable influenza vaccines, particularly in the face of seasonal outbreaks and pandemic threats. Also, concerns about egg allergies and limitations in egg supply have prompted a shift towards cell-based production methods.
In early 2024, investigators from Taiwan’s National Institute of Infectious Diseases and Vaccinology revealed a report on a predictive model developed to assess the cost-effectiveness of quadrivalent flu vaccines produced via cell-based technology, versus those manufactured using egg-based methods. In comparison to egg-based quadrivalent influenza vaccines, the analysis demonstrated that using cell-based vaccines would prevent approx. 15,665 flu cases, 2,244 complicated cases, and nearly 260 hospitalizations every year.
Although the total cost of vaccination was estimated to be around US$4.5 million higher with cell-based vaccines, the cost of treating flu infections among pediatric patients would reduce by roughly US$990,000 annually. As evident, by opting for cell-based quadrivalent flu vaccines, we can save on treatment costs while reducing the cases of flu and its associated complications.
Universal Flu Vaccine Research
Universal flu vaccine research has been gaining momentum in recent years, with notable progress being made towards developing a vaccine that can provide broad protection against multiple strains of the influenza virus. Recent advancements include promising preclinical and clinical trials demonstrating the potential efficacy of novel vaccine candidates. For example, researchers have developed vaccines that target the stalk region of the influenza virus’s hemagglutinin protein, which is highly conserved across different influenza strains.
Clinical trials evaluating these vaccines have shown encouraging results, with some candidates eliciting broad and durable immune responses in human subjects.
A significant development in the field of universal influenza vaccine research is the ongoing work of the Collaborative Influenza Vaccine Innovation Centers (CIVICs) program, which was created in 2019 to support the development of broadly protective and longer-lasting flu vaccines. The program aimed to improve our understanding of the immune response to influenza viruses and develop innovative approaches to vaccine design.
An example of a more recent progress is a clinical trial of an mRNA universal influenza vaccine candidate developed by researchers at NIAID Vaccine Research Center, which began in May 2023. This vaccine aims to target six flu strains and could serve as an important line of defense against future flu pandemics. Continued investment and support for universal flu vaccine research are essential to address the evolving nature of influenza viruses and protect global populations from the ongoing threat of the virus.
Flu Vaccination Coverage Rates in the U.S.
Influenza vaccination coverage tends to be lower among healthy adults under 65 compared to older adults and those with certain medical conditions, as per the CDC. Coverage among children and healthcare workers is higher on average. There are also disparities in flu vaccination coverage based on factors like race, ethnicity, education level, and access to healthcare. Work still needs to be done to improve vaccination rates and reduce gaps between populations. Widespread flu vaccination coverage each year as an important public health goal will augment the influenza vaccines industry scope.
Barriers to Vaccination
Despite the demonstrated benefits of flu vaccination, vaccination rates remain low in the United States and globally. There are several key barriers that continue to impede higher vaccination rates:
Misconceptions about safety and efficacy– Common misconceptions about the flu vaccine include that it causes the flu, it is not effective, or that it has dangerous side effects. A 2023 survey conducted by NFID on Influenza, COVID-19, Respiratory Syncytial Virus, and Pneumococcal Disease from 1,000 responses affirmed that among the people who did not want to take flu vaccinations or were unsure, 31% did not trust the vaccines while 27% expressed concerns regarding vaccine-induced illness.
Lack of awareness – Many people take lightly the risks of influenza, the need for vaccines, or recommendations around who should get vaccinated. Increased public education and awareness campaigns from public health organizations could help address this.
Lack of access– Vaccine access issues disproportionately affect minority groups, low-income populations, and developing regions globally. Barriers like high costs, lack of transportation, inability to take time off work, or simply lack of availability in certain areas reduce vaccination coverage.
Efforts to increase access through free vaccination programs, expanded clinic hours, mobile vaccination drives, and low-cost or publicly funded vaccine doses could improve coverage among affected demographics, strengthening the regional influenza vaccines market. For instance, the CDC’s “Wild to Mild” campaign launched in September last year was initiated to spread critical information regarding the importance of influenza vaccine and how it can lower the risk of serious outcomes from the virus.
Flue Vaccination among Nursing Home Residents
In the United States, there are more than 26,000 nursing home facilities. Nursing homes house a significant portion of age group more vulnerable to influenza virus, making them a crucial focus for flu prevention efforts.
While flu vaccination is strongly recommended by the CDC for all adults 65 and older, including those in nursing homes, the reality paints a less optimistic picture. According to a 2023 CDC report, the 2022-23 flu season saw a vaccination rate of only 42.2% among nursing home residents in the country, suggesting a key challenge to overcome for the U.S. influenza vaccines industry.
There can be several factors that contribute to low influenza vaccination rates in nursing homes, such as:
Misconceptions about the flu vaccine’s effectiveness and safety.
Difficulty vaccinating cognitively impaired residents who cannot consent.
Lack of vaccination requirements for healthcare workers in long-term care facilities.
Failure to stock adequate flu vaccine supplies.
The consequences of low vaccination rates can be dire, as nursing home residents are at increased risk of severe complications from flu, including pneumonia, hospitalization, and even death. A 2022 study published in the Journal of the American Geriatrics Society found that unvaccinated residents were over five times more likely to be hospitalized due to flu compared to vaccinated individuals.
By understanding the current state of flu vaccination rates in nursing homes, acknowledging the contributing factors, and exploring potential solutions, we can work towards better protecting our vulnerable elders. Through targeted education, open communication, and streamlined processes, we can empower residents, families, and healthcare professionals to make informed decisions and prioritize flu protection.
Influenza is a serious public health threat that causes severe illness, hospitalization, and death every year. The influenza vaccines available today are safe and effective. Getting an annual flu shot protects you and the whole community. Targeted education in the industry will involve delivering easily understandable and culturally relevant information to residents, families, and healthcare staff to underscore the significance and advantages of vaccination. Streamlining logistics by working closely with healthcare providers and facilities to simplify vaccination procedures, such as organizing on-site clinics and resolving transportation obstacles, will bolster the North America influenza market outlook.